http://www.jocr.co.in/wp/2013/07/10/2250-0685-109-fulltext/
Progressive Brachial Plexus Palsy after Osteosynthesis of an Inveterate Clavicular Fracture
Posted on Jul 10, 2013 in July - Sep 2013, Volume 3 Issue 3
What to Learn from this Article?
What to Learn from this Article?
Unique scenario of progressive brachial plexus palsy following osteosynthesis of clavicle
Case Report | Volume 3 | Issue 3 | JOCR July-Sep 2013 | Page 18-21 | Rosati M, Andreani L, Poggetti A, Zampa V, Parchi P, Lisanti M.
Authors: Rosati M[1], Andreani L[1], Poggetti A[1], Zampa V[2], Parchi P[1], Lisanti M[1]
[1]Orthopaedic and Traumatology I Department, University of Pisa.
[2]Diagnostic I Department, University of Pisa.
Address of Correspondence:
Dr Marco Rosati: Orthopaedic and Traumatology I Department, University of Pisa 050/996504 050/996501 (fax). Email: rosati1961@gmail.com.
Abstract
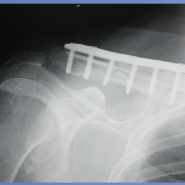
Introduction: The thoracic outlet syndrome (TOS) is a rare complication of clavicular fracture, occurring in 0.5-9% of cases . In the literature from 1965 – 2010, 425 cases of TOS complicating a claviclular fracture were described. However, only 5 were observed after a surgical procedure of reduction and fixation. The causes of this complication were due to the presence of an exuberant callus, to technical surgery errors or to vascular lesions. In this paper we describe a case of brachial plexus plasy after osteosynthesis of clavicle fracture.
Case Report: A 48 year old female, presented to us with inveterate middle third clavicle fracture of 2 months duration. She was an alcoholic, smoker with an history of opiate abuse and was HCV positive. At two month the fracture was displaced with no signs of union and open rigid fixation with plate was done. The immediate postoperative patient had signs of neurologic injury. Five days after surgery showed paralysis of the ulnar nerve, at 10 days paralysis of the median nerve, radial and ulnar paresthesias in the territory of the C5-C6-C7-C8 roots. She was treated with rest, steroids and neurotrophic drugs. One month after surgery the patient had signs of complete denervation around the brachial plexus. Implant removal was done and in a month ulnar and median nerve functions recovered. At three months post implant removal the neurological picture returned to normal.
Conclusion: We can say that TOS can be seen as arising secondary to an “iatrogenic compartment syndrome” justified by the particular anatomy of the space cost joint. The appropriateness of the intervention for removal of fixation devices is demonstrated by the fact that the patient has returned to her daily activities in the absence of symptoms and good functional recovery in about three months, despite fracture nonunion.
Keywords: Brachial plexus palsy, clavicle fractures, outlet thoracic syndrome.
Authors Reply: Progressive Brachial Plexus Palsy after Osteosynthesis of an Inveterate Clavicular Fracture
Posted on Jan 16, 2014 in Jan - Mar 2014, Volume 4 Issue 1
Letter to Editor
Volume 4 | Issue 1 | JOCR Jan-Mar 2014 | Page 44 |
Rosati M, Andreani L, Poggetti A, Zampa V, Parchi P, Lisanti M
Authors Reply:Progressive Brachial Plexus Palsy after Osteosynthesis of an Inveterate Clavicular Fracture-
Authors: Rosati M[1], Andreani L[1], Poggetti A[1], Zampa V[2], Parchi P, Lisanti M
[1]Orthopaedic and Traumatology I Department, University of Pisa.
[2]Diagnostic I Department, University of Pisa.
Address of Correspondence:
Dr Marco Rosati: Orthopaedic and Traumatology I Department, University of Pisa 050/996504 050/996501 (fax). Email: rosati1961@gmail.com.
Dear sir,
First of all I want to say thank you for your questions [1] about our article [2] as it allows us to give some clarifications for better understanding of our paper:
1. The fracture was operated 4 months later the injury. The abstract report about 2 months later the injury is a mistake. About point 2,3 and 4 we think that the only explanation for the symptoms onset was narrowing of the virtual space where brachial plexus lies. No excessive screws length, neither exuberant callus, neither an hematoma were discovered during the plate removal. We only remolded the stumps of clavicle. 5. The fracture was fixed again because medial stump cause a skin ulcer. We preferred the plate because it allowed the curettage of the non-union site. We did not use other types of synthesis (intramedullary nail, etc), indeed it was a difficult case of nonunion.
Thank you and best wishes.
Rosati M, Andreani L, Poggetti A, Zampa V, Parchi P, Lisanti M.
Orthopaedic and Traumatology I Department, University of Pisa.
Diagnostic I Department, University of Pisa.

No hay comentarios:
Publicar un comentario